Lumbar Herniated Disc
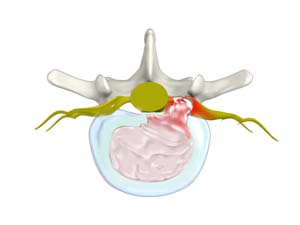
Herniated disc is a condition in which the outer fibers (annulus) of the intervertebral disc are damaged causing the soft inner material of the nucleus pulposus to rupture out of its space. A herniated disc, common in the lower back (lumbar spine) occurs when there is a tear in the outer lining of the disc (annulus fibrosus). This causes the inner jelly-like material (nucleus pulposus) to leak out and place pressure on the adjacent spinal nerve root. It is the most common cause of low back pain and pain that radiates down the leg (radiculopathy).
The most common signs and symptoms of lumbar disc herniation are back pain that radiates to buttocks and legs, numbness in the leg or foot, weakness in the leg or foot, and rarely, loss of bowel and bladder control.
Diagnosis
Proper diagnosis of the condition requires a complete medical history and a careful physical examination by your physician. Some of the additional diagnostic tests your doctor may suggest include:
- X-ray of the middle-back: X-rays help to detect the amount of wear and tear present and to rule out other conditions.
- CT and MRI scan: These tests are done to confirm the diagnosis of herniated disc.
Treatment Options
Conservative Treatment
Conservative treatment includes pain medications, physical therapy, and avoiding strenuous activity if the pain is severe.
Epidural Steroid Injection (ESI): ESI can be considered if the pain is intolerable even with medications and rest.
Surgical Treatment
Lumbar microdiscectomy is a surgical procedure done to remove a herniated part of the disc and any fragments that are putting pressure on the spinal nerve. This surgical procedure involves use of a surgical microscope and microsurgical techniques to gain access to the lumbar spine. The microscope magnifies and illuminates the area of operation. Only a small portion of the herniated disc that pinches on the nerve roots is removed.

